Advanced Approaches to Liver Cancer and Metastasis Treatment
- Sarah Mitchell

- Jul 30, 2025
- 13 min read
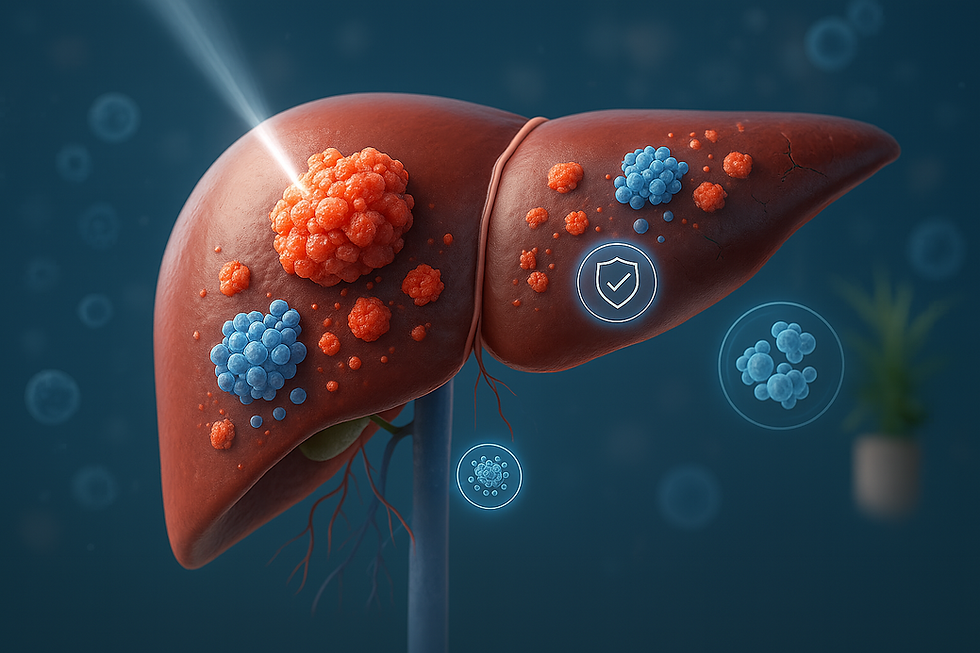
Treating liver cancer and its metastases presents one of the most intricate challenges in modern medicine. As the sixth most common cancer globally, with over 866,000 new cases diagnosed in 2022, its diverse forms and the potential for spread from other organs make it a complex condition for both patients and healthcare providers.
A particularly critical aspect is liver metastasis, where cancer cells from other parts of the body spread to the liver. Certain cancers, such as colorectal or lung cancer, show a strong tendency to form liver metastases. For instance, up to 70% of individuals with colorectal cancer may eventually develop liver metastases. When liver involvement occurs in stage 4 metastatic cancer, it often indicates a severe and challenging prognosis. This reality has driven the medical community to innovate, developing specialized treatment programs that aim not just for palliative care, but for effective cancer control and, in some cases, even the potential for a cure.
Understanding Liver Cancer and Metastasis
The liver can be affected by cancer in two primary ways:
Primary vs. Secondary Liver Cancer
Primary liver cancer originates directly in the liver. The most common type is hepatocellular carcinoma, which develops from hepatocytes, the liver's main cells. Other less common primary liver cancers include cholangiocarcinoma, angiosarcoma, and hepatoblastoma, arising from different liver cells and structures.
Secondary liver cancer (liver metastasis) occurs much more frequently. This happens when cancer cells from other organs travel to the liver through the bloodstream or lymphatic system and form new tumors.
Common Cancers That Spread to the Liver
Several types of cancer commonly lead to secondary tumors in the liver:
Colorectal Cancer: Accounting for approximately 50% of metastatic liver cancer cases, this is due to the fact that blood from all unpaired abdominal organs flows into the liver via the portal vein, making it a common site for spread.
Breast Cancer: Around 30% of women with advanced breast cancer develop liver metastases.
Lung Cancer: Roughly 30% of patients diagnosed with lung cancer show evidence of liver metastases on imaging scans like CT or MRI.
Upper Gastrointestinal Tract Cancers: This includes cancers of the stomach and esophagus. Spread to the liver can occur through both lymphatic and blood vessels, as well as direct contact, with liver metastasis rates ranging from 10% to 40%.
Pancreatic Cancer: Due to the liver's unique blood supply, up to 50% of patients with pancreatic cancer may also have liver metastases.
Given the liver's vital role as a detoxification organ, receiving blood from all parts of the body, it is crucial to perform abdominal CT/MRI scans in any advanced cancer diagnosis to rule out the presence of liver metastases.
Traditional and Evolving Treatment Strategies
Historically, the primary approach for treating both primary liver cancer and liver metastases involved surgery combined with chemotherapy (which could be regional or systemic, and administered before, during, or after surgery). The most favorable outcomes were typically seen when all malignant foci could be completely removed.
Challenges in Liver Cancer Surgery
Surgeons often face significant obstacles when operating on advanced primary or metastatic liver cancer, including:
Extensive Tumor Spread: The cancer may have spread so widely throughout the liver that very little healthy organ tissue remains. Due to the liver's active blood flow, metastases frequently affect both lobes.
Compromised Liver Function: Prior chemotherapy or other long-term treatments can reduce liver function.
Underlying Liver Conditions: Pre-existing conditions like cirrhosis or hepatitis, or age-related changes, can further impair liver function.
In the past, patients with widespread metastatic liver disease often had limited options beyond palliative care aimed at symptom relief. Controlling the cancer or significantly increasing life expectancy seemed out of reach. However, the landscape of treatment began to change dramatically with the introduction of two-stage liver splitting surgery, known as ALPPS.

The Breakthrough of ALPPS Surgery
The advent of ALPPS (Associated Liver Partition and Portal Vein Ligation for Staged Hepatectomy) surgery has revolutionized the treatment of complex liver tumors. This innovative procedure has expanded the possibilities for radical treatment of liver tumors and metastases that were previously considered unresectable or only conditionally resectable, offering new hope for recovery. Surgeons are no longer confined to traditional anatomical resections, as ALPPS can be successfully performed even for lesions affecting both liver lobes and when less than 25% of healthy liver parenchyma is initially preserved.
Principles of Curative Liver Cancer Treatment
The liver possesses an extraordinary capacity for regeneration. It can fully restore its volume and normal function, provided that at least 25% of healthy parenchyma remains after surgical removal of diseased tissue. This remarkable ability empowers surgical oncologists to undertake interventions that might otherwise seem impossible.
The Liver's Regenerative Power
The liver's unique ability to regrow itself is a cornerstone of advanced surgical strategies. This regenerative capacity is what makes complex, multi-stage procedures like ALPPS feasible, allowing surgeons to remove large portions of diseased liver while ensuring the patient's long-term liver function.
Goals of Radical Surgical Intervention
Curative (radical) surgical treatment for primary and secondary malignant liver tumors adheres to two fundamental principles:
Total Removal of Malignant Foci: This involves the complete excision of all cancerous tissues within the liver, along with any affected regional lymph nodes and adjacent organs.
Preservation of Normal Liver Function: Ensuring the liver can perform its vital roles post-surgery, including detoxification, participation in metabolism, synthesis of blood clotting factors, and bile production for fat absorption.
Adhering to these principles becomes particularly challenging when cancer has spread to both lobes of the liver. If a surgeon were to remove all affected tissues in a single procedure, the patient would likely suffer from life-threatening liver failure.
ALPPS: Expanding Surgical Possibilities
The ALPPS procedure is designed to meet these stringent requirements. This two-stage surgical intervention significantly broadens the scope of radical treatment for liver tumors and metastases that were previously considered inoperable or borderline resectable. It offers patients a chance at recovery by enabling surgeons to overcome the limitations of traditional anatomical resections, even in cases of bilobar lesions where less than 25% of healthy liver parenchyma might initially be preserved.
The ALPPS Surgical Procedure: A Detailed Look
The success of any surgical intervention, especially one as complex as ALPPS, relies heavily on meticulous planning.
Preoperative Planning and Assessment
Before surgery, a thorough preparation phase is essential, typically including:
Imaging Tests: Ultrasound, CT, and MRI scans are performed to precisely evaluate the primary tumor's characteristics, the number and size of liver metastases, and to identify any fibrotic changes or steatosis (fatty liver).
Laboratory Liver Function Tests: Blood tests are conducted to assess liver health, including levels of transaminases, bilirubin fractions, LDH, alkaline phosphatase, and protein fractions.
Infection Screening: Blood tests for various types of hepatitis and AIDS are also part of the preoperative workup.
During the planning stage, surgeons meticulously assess the volume of the future liver remnant (FLR) and its functional reserve. Modern computer programs, often supplementing clinical experience, aid doctors in this crucial assessment. For example, software developed by teams like Fraunhofer MEVIS analyzes imaging data using sophisticated mathematical models, providing insights that allow surgeons to confidently proceed with complex surgeries while prioritizing patient safety.
Stage One: Preparing the Liver for Regeneration
The first stage of the ALPPS operation typically lasts up to three hours. It involves:
Liver Splitting: The liver is either totally or partially split along the falciform ligament, extending to the retrohepatic segment of the inferior vena cava.
Portal Vein Ligation/Embolization: The right portal vein branch is then embolized or ligated.
Left Lobe Sanitization: The surgeon ensures the left lobe of the liver is free of any malignant foci, even microscopic ones.
Following this stage, the blockage of blood flow in part of the portal vein initiates the liver's regeneration process, leading to hypertrophy (enlargement) of the healthy liver tissue.
Stage Two: Completing the Resection
The second stage of the operation is performed once the healthy liver parenchyma has sufficiently hypertrophied and liver function test parameters have returned to normal levels. This indicates that the liver's functional reserve is adequate for the final stage: an extended right hemihepatectomy and removal of regional lymph nodes. The time between the two surgical procedures can vary, typically ranging from 1-2 weeks to 1-1.5 months, with the surgical team individually tailoring the optimal timing for each patient.
Postoperative Care and Recovery
Postoperative care is critical for ensuring a patient's successful recovery and long-term well-being after liver cancer surgery.
Goals of Postoperative Care
The medical team focuses on several key objectives during the postoperative period:
Liver Function Assessment: Ensuring the liver's functional reserve is normal and preventing liver failure.
Tumor Control Verification: Confirming the radicality of the treatment and monitoring for any signs of tumor growth.
Symptomatic Treatment and Rehabilitation: Providing care to improve the patient's general health and planning rehabilitation as needed.
Immediate Post-Surgery Recovery
Patients typically spend the first day after surgery in the intensive care unit, where vital signs are continuously monitored. In specialized clinics, this intensive monitoring is quickly followed by patient activation. Patients are transferred to a regular room and encouraged to gradually increase their movement and expand their diet. This active approach promotes more vigorous hypertrophy of the remaining hepatic parenchyma, facilitating a smoother and faster recovery.
Ongoing Management and Follow-Up
During the postoperative period, the oncology team may recommend one or more courses of chemotherapy. Upon discharge from the hospital, patients receive detailed instructions on nutrition, medication intake, and the schedule for follow-up examinations. Regular monitoring is essential to track recovery and detect any potential recurrence.
Integrated Approaches to Liver Cancer Management
Modern treatment for metastatic liver cancer often achieves the best outcomes when surgery is combined with other advanced therapies. This comprehensive approach targets cancer cells through multiple pathways, addressing both the primary tumor and any microscopic cancer cells that may have spread throughout the body.
Transarterial Chemoembolization (TACE): Targeted Drug Delivery
For liver tumors that cannot be surgically removed due to their size, location, or underlying liver conditions like cirrhosis, transarterial chemoembolization (TACE) offers a highly targeted treatment. This procedure allows physicians to deliver concentrated chemotherapy drugs directly to liver tumors while minimizing exposure to healthy tissues throughout the body.
During TACE, a thin catheter is inserted through a blood vessel in the groin and carefully guided to the hepatic artery, which supplies blood to the liver tumor. Once positioned, chemotherapy drugs are injected directly into the tumor's blood supply. This is followed by the injection of tiny particles called emboli, which block the blood vessel. This blockage serves a dual purpose: it traps the chemotherapy within the tumor for maximum effect and cuts off the tumor's vital oxygen and nutrient supply.
The advantages of TACE over traditional systemic chemotherapy include:
Higher Drug Concentration: Delivers chemotherapy doses up to 15 times higher directly to the tumor.
Reduced Side Effects: Limits chemotherapy exposure to healthy organs throughout the body, reducing systemic side effects.
Extended Tumor Control: Blocks the blood supply, effectively starving the tumor of oxygen and nutrients.
Preserved Liver Function: Protects healthy liver tissue from unnecessary chemotherapy damage.
Recent clinical trials have demonstrated that combining TACE with newer immunotherapy and anti-angiogenesis drugs can significantly extend progression-free survival, with patients experiencing 14-15 months of progression-free survival compared to 8-10 months with TACE alone.

Hyperthermia: Harnessing Heat to Combat Cancer
Hyperthermia therapy utilizes precisely controlled heat to treat liver metastases, offering an innovative option for patients whose cancer cannot be surgically removed or for those looking to enhance their existing treatments. This thermal therapy raises tumor temperatures to between 104-113°F (40-45°C), exploiting the increased sensitivity of cancer cells to heat compared to healthy tissue.
The procedure can involve different approaches based on tumor location and size:
Local Hyperthermia: Uses radiofrequency ablation (RFA), where a thin needle is inserted directly into the tumor under imaging guidance. The probe delivers high-frequency energy, creating targeted heat that destroys cancer cells within a specific area.
Regional Hyperthermia: Can heat larger sections of the liver and is often combined with chemotherapy or radiation therapy.
The benefits of hyperthermia for patients with secondary liver cancer are notable:
Enhanced Treatment Effectiveness: May increase the success rates of chemotherapy and radiation therapy by 30-50%.
Improved Drug Delivery: Increased blood flow due to heat allows chemotherapy to penetrate deeper into tumors that have spread to the liver.
Immune System Activation: Heat can trigger immune responses, helping the body recognize and attack cancer cells.
Minimal Side Effects: Precisely targeted treatment helps protect surrounding healthy liver tissue.
Research indicates that combining hyperthermia with radiation therapy can increase complete response rates in liver tumors. This treatment is particularly valuable for tumors smaller than 2 inches and can be repeated if cancer recurs. Most procedures are performed on an outpatient basis, allowing patients to maintain their quality of life while maximizing treatment effectiveness.
Dendritic cell vaccination represents a sophisticated approach to cancer immunotherapy, building on the groundbreaking research that earned Ralph Steinman the Nobel Prize in Physiology or Medicine in 2011 for his discovery of dendritic cells and their crucial role in immunity. These specialized immune cells act as powerful coordinators, identifying cancer cells and training other immune cells to target and destroy them.
The treatment process involves:
Blood Collection: Approximately 150-200ml of the patient's blood is collected.
Cell Extraction and Culture: Dendritic cells are extracted from the blood and cultured in specialized laboratories for about one week.
Personalized Vaccine Creation: During this time, the cells are "educated" using antigens from the patient's specific cancer, creating a personalized vaccine tailored to the tumor's unique characteristics. The entire process adheres to strict regulatory oversight to ensure the highest safety standards.
Key advantages of dendritic cell vaccination include:
Potential for Long-Lasting Immunity: A single injection may boost the immune system's anti-cancer response for years.
Personalized Treatment: Vaccines are custom-made using the patient's own cells and tumor-specific antigens.
Minimal Side Effects: The therapy leverages the body's natural immune mechanisms, avoiding the harsh side effects associated with toxic chemicals.
Complementary Therapy: It can be used alongside chemotherapy, radiation, and surgery without interference.
For patients with primary cancer and secondary liver cancer, dendritic cell therapy has shown promise in constraining tumor growth and extending survival, particularly when conventional options have been exhausted or are not suitable. This treatment is especially valuable for patients with liver metastases from other cancers or those requiring palliative care.
Choosing a Leading Medical Center for Liver Cancer Treatment
When faced with a liver cancer diagnosis, selecting the right treatment center is a pivotal decision. Clinical studies consistently show that advanced procedures like ALPPS surgery can lead to excellent long-term outcomes for patients with extensive liver lesions, multiple secondary cancer sites, or underlying conditions such as hepatitis or cirrhosis. These complex surgical interventions demand surgeons with exceptional skill in delicately isolating blood vessels while preserving the function of healthy liver tissue.
Why Specialized Centers Matter
The foundation of successful primary and secondary liver cancer treatment lies in access to a multidisciplinary team. This team typically includes experienced hepatobiliary surgeons, interventional radiologists, medical oncologists, and specialized nursing staff. European medical centers, particularly those in Germany, have established themselves as global leaders in comprehensive liver cancer care, integrating cutting-edge technology with decades of clinical expertise.
The Multidisciplinary Approach
A multidisciplinary team ensures that every aspect of a patient's condition is considered, leading to a tailored and effective treatment plan. This collaborative approach is crucial for managing complex cases of liver cancer and metastases, optimizing outcomes and improving liver cancer survival rates.
Key Considerations for International Treatment
If you are considering treatment abroad, it is wise to thoroughly research hospitals, review physician credentials, and understand treatment success rates to make an informed decision about your care. Many patients find it beneficial to compare various treatment options, from comprehensive programs that cover initial diagnosis through rehabilitation, to specific procedures like ALPPS surgery, TACE, or immunotherapy.
When evaluating treatment centers, consider factors such as:
The hospital's specific experience with your condition.
The availability of advanced treatment options.
Language support services.
Coordination of care for international patients.
Many specialized clinics offer assistance with medical record review, treatment plan development, and logistical support, allowing patients to focus on their recovery rather than administrative concerns. Remember that choosing the right treatment center is a deeply personal decision that should align with your medical needs, comfort level, and treatment goals.
Navigating Your Treatment Journey with Doctoury
Navigating complex liver cancer treatment decisions can feel incredibly overwhelming, especially when dealing with advanced disease or multiple treatment failures. With numerous specialists offering differing opinions and treatment protocols varying significantly between medical centers, patients often struggle to identify the most effective approach for their specific situation.
The Challenge of Complex Diagnoses
Patients facing metastatic liver cancer or other complex liver conditions deserve access to the most advanced therapeutic interventions, precisely tailored to their unique clinical circumstances, rather than settling for standard protocols or the first available options. This is where specialized medical expertise becomes invaluable.
Doctoury's Role in Advanced Care
Doctoury has dedicated over 12 years to connecting patients with innovative liver cancer treatments, developing comprehensive expertise in complex hepatobiliary cases. Our medical coordinators are deeply knowledgeable about the nuances of ALPPS surgery candidacy, TACE procedure selection, and the integration of immunotherapy for liver metastases management.
Comprehensive Support from Doctoury
For patients considering advanced liver cancer treatment abroad, Doctoury provides extensive support, including:
Assessment and detailed analysis of medical reports.
Development of a personalized medical care program.
Selection of the most suitable treatment location.
Preparation and forwarding of medical documents to the chosen clinic.
Preparatory consultations with clinicians to finalize the medical care program.
Expert advice and support during your hospital stay.
Follow-up care upon your return to your home country after completing the medical care program.
Handling all necessary formalities related to preparing for the medical care program.
Coordination and organization of your stay in a foreign country.
Assistance with visas and travel tickets.
A personal coordinator and interpreter offering 24/7 support.
Transparent budgeting with no hidden costs.
When facing liver cancer or liver metastases, your treatment decisions can significantly impact both liver cancer survival rates and overall quality of life. Partnering with experienced medical coordinators who understand the complexities of advanced hepatobiliary treatments ensures that you receive personalized care tailored to your specific needs. Contact our medical consultant to learn more about the possibilities of treatment with innovative methods for liver cancer and liver metastases with leading specialists in this field.
Frequently Asked Questions (FAQs)
What are the latest treatments for liver cancer?
The newest treatments for liver cancer and metastases include ALPPS two-stage surgery for complex cases, Transarterial Chemoembolization (TACE) for targeted chemotherapy delivery, hyperthermia therapy using controlled heat, and dendritic cell vaccination, which trains your immune system to fight cancer cells.
Can liver metastases be treated without surgery?
Yes, non-surgical options for liver metastases include TACE, hyperthermia, and immunotherapy with dendritic cells. These treatments can help control tumor growth and potentially extend survival, especially when surgery is not a viable option.
What are some common liver cancer symptoms?
Common liver cancer symptoms can include unexplained weight loss, loss of appetite, nausea, vomiting, fatigue, an enlarged liver (felt as fullness under the right ribs), an enlarged spleen, pain in the upper abdomen, swelling or fluid buildup in the abdomen, jaundice (yellowing of skin and eyes), and dark urine. These symptoms can also be caused by other conditions, so a medical evaluation is essential.
Where can I receive innovative liver cancer treatments?
Leading clinics in Europe, particularly in Germany, offer comprehensive liver cancer programs with advanced procedures like ALPPS surgery, TACE, and immunotherapy. These specialized centers provide multidisciplinary teams and cutting-edge technology for complex cases. Doctoury can assist in connecting you with such centers.
What is the benefit of undergoing treatment abroad?
Treatment abroad provides access to specialized oncology centers with extensive experience in complex procedures, advanced technology, multidisciplinary care teams, and comprehensive support services for international patients throughout their treatment journey. This can include access to treatments not readily available in one's home country.




Comments